Medical Billing & Coding
With several years of expertise on both physician and reimbursement sides, our highly qualified and dedicated team of CPC and CPC-H outpatient facility certified coders from American Academy of Professional Coders (AAPC) ensure highly accurate and compliant coding services. We have got an extremely well qualified coders and trainers oversee daily operation of our Coding department and see to it that all levels of claims is audited prior to transmission of claims or needs are met.
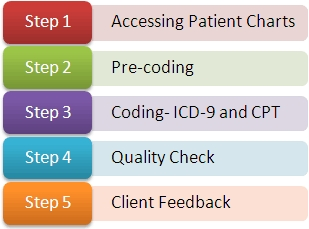
The coding process includes the following steps:

- Patient demographics, policy details, files that are electronically scanned at our physician’s office are securely accessed by our billing team following HIPAA rules.
- Our teams verify and validate the documents, split them into batches and review them until the needs of the claims are met.
- Diagnosis, Procedure Codes and modifiers are assigned to support the codes as per the insurance guidelines.
- Modification of certain codes may be made as per carrier requirement. Our expert auditors and oriented quality control team audit the coded charge sheets and process it further for charge entry and cash posting.
We use the following industry coding standards:

Diagnosis Codes (ICD-9: International Classification of Disease)
Procedure Codes (CPT-4: Current Procedural Terminology)
Coding for Inpatient Services (ICD-9)
Drug Codes (NDC: National Drug Codes)
Other Procedure Codes (HCPCS: Healthcare Common Procedure Coding System)








